The Challenge
Property and Casualty – Payment Integrity
MultiPlan analysis showed a property and casualty servicer how it could strengthen its bill review and network services by:
- Using analytics tuned to find wasteful or abusive medical billing practices not identifiable by more automated bill review programs
- Implementing resolution strategies appropriate for the severity of issues and nature of the provider relationships

The Solution
MultiPlan is enabling a comprehensive payment integrity program to complement existing bill review:
- In place: Clinical Negotiation – clinically-driven negotiation of non-contracted bills scoring high for potential waste or abuse
- In process: Advanced Code Editing – identification and denial of charges in error, for both contracted and non-contracted bills with evidence of issues missed by the primary editing process
The Results
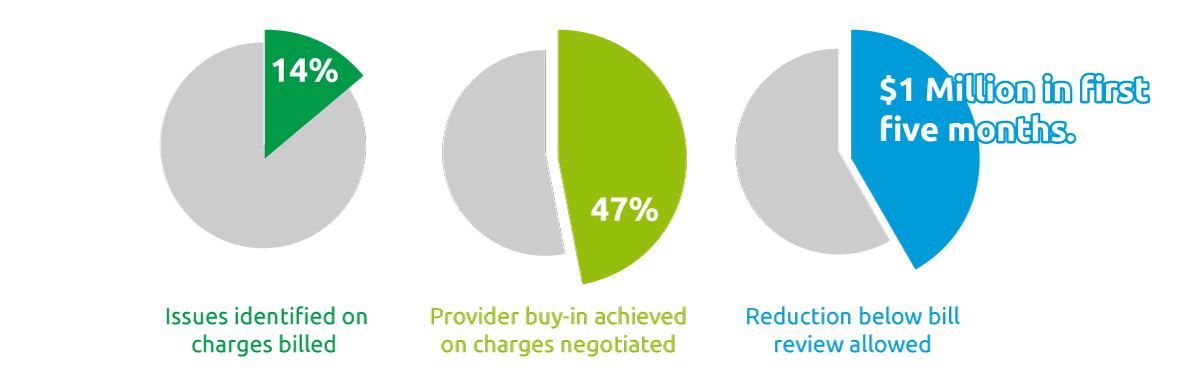
From the program’s start, MultiPlan Clinical Negotiation has generated significant additional medical cost reduction:
- Identifying issues on 14% of charges billed
- Achieving provider buy-in on 47% of charges negotiated
- Passing the $1 million mark for reduction below bill review allowed, within the first five months